The posterior auricular nerve is a crucial part of the human nervous system that plays a significant role in both sensory perception and motor functions. To fully comprehend the importance of this nerve, it’s essential to delve into its anatomy, function, and clinical significance. In this article, we will explore the intricate details surrounding the posterior auricular nerve and its role in maintaining our overall health and well-being.
Anatomy of the Posterior Auricular Nerve
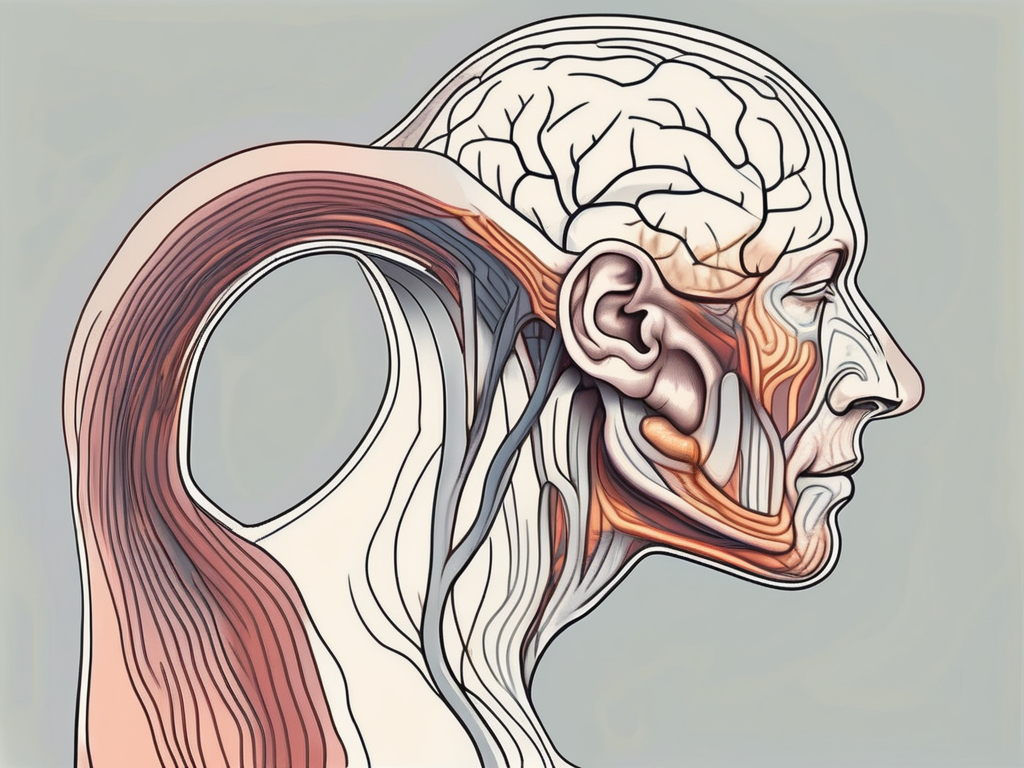
The posterior auricular nerve is a branch of the facial nerve, specifically arising from the auriculotemporal nerve. It passes through the parotid gland, an essential gland responsible for producing saliva, before branching out into various interconnected pathways within the scalp and the upper part of the face.
As a sensory nerve, the posterior auricular nerve supplies sensation to the posterior part of the auricle, the region behind the ear, and the area surrounding the mastoid process, which is the prominent bony projection located just behind the ear.
The posterior auricular nerve plays a crucial role in the intricate network of nerves that contribute to the complex sensory innervation of the head and face. It is responsible for transmitting sensory information from the posterior auricle and the mastoid process, allowing us to perceive touch, pressure, and temperature in these areas.
Originating from the auriculotemporal nerve, which arises from the mandibular division of the trigeminal nerve, the posterior auricular nerve follows a fascinating pathway through the parotid gland.
Origin and Pathway of the Posterior Auricular Nerve
The posterior auricular nerve originates from the auriculotemporal nerve, which arises from the mandibular division of the trigeminal nerve. It traverses through the parotid gland, where it divides into several branches that innervate different areas.
One branch of the posterior auricular nerve continues its course through the temporoparietal fascia, supplying sensory fibers to the scalp and the skin posterior to the ear. This intricate pathway allows for the transmission of sensory information from the scalp, enabling us to perceive sensations such as touch, pressure, and pain in this region.
Another branch of the posterior auricular nerve joins the greater auricular nerve, which provides sensation to the lower part of the auricle. This connection ensures comprehensive sensory innervation of the auricle, allowing us to perceive touch, pressure, and temperature in this area.
Branches and Connections of the Posterior Auricular Nerve
Within the parotid gland, the posterior auricular nerve communicates with the auriculotemporal nerve, the facial nerve, and the external carotid plexus, forming an intricate network of neural connections. These connections facilitate the transmission of sensory information and enable coordinated motor functions.
The posterior auricular nerve’s connections with the auriculotemporal nerve and the facial nerve are particularly significant. These connections allow for the integration of sensory and motor functions, ensuring the proper functioning of facial expressions and the perception of sensory stimuli in the head and face.
In addition to its connections within the parotid gland, the posterior auricular nerve also displays interconnectedness with the lesser occipital nerve and the greater occipital nerve. These connections contribute to the complex sensory innervation of the scalp, allowing us to perceive touch, pressure, and pain in this region.
The intricate network of branches and connections of the posterior auricular nerve highlights its role in sensory perception and motor coordination in the head and face. Understanding the anatomy of this nerve provides valuable insights into the complex functioning of the human nervous system.
Function of the Posterior Auricular Nerve
As mentioned before, the posterior auricular nerve serves both sensory and motor functions. Let’s explore each of these functions in detail.
Role in Sensory Perception
The posterior auricular nerve is primarily responsible for transmitting sensory information from the posterior part of the auricle and the surrounding structures to the brain. This includes detecting touch, temperature, pain, and pressure.
When you touch the back of your ear, the posterior auricular nerve sends signals to your brain, allowing you to feel the sensation. Similarly, when you experience a change in temperature, such as a cool breeze on your ear, the nerve relays this information to your brain, helping you perceive the difference.
If you accidentally prick the back of your ear with a sharp object, the posterior auricular nerve quickly sends pain signals to your brain, alerting you to the injury. This rapid transmission of pain information is crucial for your body’s protective response, as it prompts you to remove the source of pain and prevent further harm.
Impairment of the sensory function of the posterior auricular nerve can result in various symptoms, such as numbness, tingling, or a loss of sensation in the affected areas. These symptoms may be caused by nerve compression, injury, or certain medical conditions.
For example, if the nerve becomes compressed due to swelling or inflammation, you may experience numbness or tingling in the back of your ear. Similarly, certain medical conditions, such as diabetes or peripheral neuropathy, can affect the function of the posterior auricular nerve, leading to sensory disturbances.
If you experience any unusual sensations or changes in the sensitivity of your ear, mastoid process, or scalp, it’s advisable to consult with a healthcare professional for a proper evaluation and diagnosis.
Contribution to Motor Functions
In addition to its sensory role, the posterior auricular nerve also contributes to motor functions. It supplies the posterior belly of the digastric muscle, which helps control the movement of the lower jaw, and the stylohyoid muscle, which plays a role in swallowing and speech.
When you chew food, the posterior auricular nerve sends signals to the posterior belly of the digastric muscle, enabling it to contract and assist in the movement of your lower jaw. This coordinated muscle action allows you to effectively break down food and facilitate the process of digestion.
The stylohyoid muscle, innervated by the posterior auricular nerve, is involved in the swallowing process. It helps elevate the hyoid bone, which in turn aids in the movement of the tongue and the passage of food from the mouth to the esophagus. Additionally, the stylohyoid muscle plays a role in speech production, contributing to the articulation of certain sounds.
Injury or damage to the posterior auricular nerve can result in weakness or paralysis of these muscles, leading to difficulties in chewing, swallowing, or speaking. For example, if the nerve is affected by trauma or compression, you may experience difficulty opening or closing your mouth properly, leading to challenges in eating or speaking.
If you experience any changes or challenges in these motor functions, it’s essential to seek professional medical assistance to determine the underlying cause. Prompt diagnosis and treatment can help restore normal function and improve your quality of life.
Clinical Significance of the Posterior Auricular Nerve
The posterior auricular nerve plays a crucial role in various clinical scenarios, making it essential for healthcare professionals to have a comprehensive understanding of its clinical significance. This knowledge enables them to accurately diagnose and effectively manage conditions related to this nerve.
The posterior auricular nerve can be affected by several disorders, each with its own set of symptoms and implications. Trauma or injury to the nerve, facial nerve disorders like Bell’s palsy, infections, tumors, or autoimmune disorders can all have an impact on the functioning of the posterior auricular nerve.
When the posterior auricular nerve is compromised, individuals may experience a range of symptoms. These can include pain, numbness, tingling, muscle weakness, inflammation, or abnormal sensations in the affected areas. Recognizing these symptoms and understanding their association with posterior auricular nerve disorders is crucial in order to seek appropriate medical attention.
Common Disorders and Symptoms
Let’s delve deeper into some of the common disorders and symptoms associated with the posterior auricular nerve.
Trauma or injury to the posterior auricular nerve can occur due to various factors such as accidents, falls, or direct blows to the head. Depending on the severity of the trauma, individuals may experience symptoms ranging from mild discomfort to severe pain and loss of function. Prompt medical evaluation and intervention are necessary to prevent further complications and promote optimal recovery.
Bell’s palsy, a facial nerve disorder, can also affect the posterior auricular nerve. This condition is characterized by sudden weakness or paralysis of the muscles on one side of the face. In some cases, individuals may experience pain or discomfort in the posterior auricular region along with other facial symptoms. Timely diagnosis and appropriate management are crucial for minimizing long-term complications and promoting facial nerve recovery.
Infections, such as otitis media or mastoiditis, can also involve the posterior auricular nerve. These infections can cause inflammation and irritation of the nerve, leading to symptoms like pain, swelling, and tenderness in the affected area. Prompt medical treatment with antibiotics or other appropriate interventions is necessary to prevent the spread of infection and alleviate symptoms.
Tumors, whether benign or malignant, can potentially affect the posterior auricular nerve. Depending on the location and nature of the tumor, individuals may experience a variety of symptoms such as pain, numbness, or muscle weakness. Early detection and appropriate management, which may involve surgical intervention or other treatments, are crucial for optimizing outcomes and preserving nerve function.
Autoimmune disorders, such as multiple sclerosis or Guillain-Barré syndrome, can also impact the posterior auricular nerve. These conditions involve the immune system mistakenly attacking the body’s own tissues, including nerves. Symptoms can vary widely and may include pain, numbness, muscle weakness, or difficulty with coordination. Timely diagnosis and appropriate management, often involving a multidisciplinary approach, are essential for minimizing disease progression and maintaining quality of life.
Diagnostic Techniques for Posterior Auricular Nerve Damage
Accurate diagnosis of posterior auricular nerve damage is vital for effective management. Healthcare professionals employ various diagnostic techniques to assess the integrity and function of the nerve.
A thorough physical examination is typically the first step in diagnosing posterior auricular nerve damage. This examination involves assessing the affected area, evaluating muscle strength and reflexes, and identifying any visible signs of nerve impairment. Additionally, a comprehensive review of the individual’s medical history helps provide valuable insights into potential underlying causes or contributing factors.
In some cases, healthcare professionals may recommend imaging studies like magnetic resonance imaging (MRI) or computed tomography (CT) scans to obtain detailed images of the affected area. These imaging techniques can help identify structural abnormalities, such as tumors or nerve compression, that may be contributing to the symptoms.
Nerve conduction studies and electromyography (EMG) are specialized tests that can assess the overall function and integrity of the posterior auricular nerve and associated muscles. Nerve conduction studies measure the speed and strength of electrical signals as they travel along the nerve, while EMG evaluates the electrical activity of the muscles. These tests can provide valuable information about the extent and location of nerve damage.
It is important to note that the choice of diagnostic techniques may vary depending on the specific clinical situation. A qualified healthcare professional will determine the most appropriate approach based on the individual’s symptoms, medical history, and physical examination findings.
In conclusion, understanding the clinical significance of the posterior auricular nerve is crucial for healthcare professionals. By recognizing the common disorders and symptoms associated with this nerve, and employing appropriate diagnostic techniques, healthcare professionals can provide accurate diagnoses and effective management strategies for individuals with posterior auricular nerve-related conditions.
Treatment and Management of Posterior Auricular Nerve Disorders
The treatment and management of posterior auricular nerve disorders depend on the underlying cause and severity of the condition. In some cases, conservative, non-surgical interventions may be sufficient, while others may require surgical interventions.
Posterior auricular nerve disorders can be caused by various factors, such as trauma, infections, inflammation, or nerve compression. The symptoms can range from mild discomfort to severe pain and functional impairment. Therefore, it is essential to seek medical advice to determine the most appropriate treatment approach.
Non-surgical Interventions
For mild cases or those caused by temporary factors like infections or inflammation, non-surgical interventions may be the primary approach. These interventions aim to alleviate symptoms, promote healing, and restore normal nerve function.
Pain management techniques, such as the use of over-the-counter or prescription medications, can help reduce discomfort and inflammation. Physical therapy may also be recommended to improve range of motion, strengthen muscles, and enhance overall function.
In addition to these interventions, healthcare professionals may suggest lifestyle modifications, such as avoiding activities that aggravate the symptoms and practicing relaxation techniques to manage stress. These non-surgical approaches can be effective in many cases and provide significant relief.
It’s important to consult with a healthcare professional to determine the most suitable non-surgical interventions for your specific condition. They will consider factors such as the cause of the disorder, the severity of symptoms, and your overall health to develop an individualized treatment plan.
Surgical Options and Outcomes
In severe cases or when conservative interventions fail to provide relief, surgical options may be considered. Surgical interventions for posterior auricular nerve disorders are typically reserved for cases where there is significant nerve damage or compression that cannot be resolved through non-surgical means.
The specific surgical approach depends on the underlying cause and the extent of nerve damage. Nerve decompression, a procedure that involves relieving pressure on the affected nerve, may be performed to restore normal nerve function. Neural repair or reconstruction techniques can also be employed to repair damaged nerves and promote regeneration.
It’s crucial to consult with a healthcare professional experienced in neurosurgery or other relevant specialties to discuss the potential risks, benefits, and outcomes of surgical interventions. They will assess your condition thoroughly, explain the surgical options available, and help you make an informed decision about the most appropriate course of action.
Recovery from surgical interventions for posterior auricular nerve disorders can vary depending on the complexity of the procedure and individual factors. Rehabilitation and post-operative care, such as physical therapy and pain management, may be necessary to optimize outcomes and ensure a successful recovery.
Follow-up appointments with healthcare professionals will be essential to monitor progress, address any concerns or complications, and adjust the treatment plan as needed. With proper care and management, many individuals with posterior auricular nerve disorders can experience significant improvement in their symptoms and quality of life.
Future Research Directions in Posterior Auricular Nerve Health
Advancements in medical research continue to shed light on the complexities of the posterior auricular nerve and its connection to overall health and well-being. Numerous future research directions hold promise for improving the understanding and management of posterior auricular nerve disorders.
The posterior auricular nerve, also known as the great auricular nerve, is a branch of the facial nerve that plays a crucial role in sensory perception and motor functions of the ear and surrounding areas. It provides innervation to the skin over the mastoid process, the auricle, and the external acoustic meatus.
One of the emerging research directions focuses on exploring innovative therapies and interventions that aim to enhance the healing and regeneration of damaged nerves, including the posterior auricular nerve. Ongoing studies investigate various approaches, such as drug therapies, gene therapies, stem cell therapies, or other novel techniques designed to promote nerve repair and restoration.
Researchers are also making significant strides in the field of diagnostic imaging techniques, which contribute to the early detection, accurate diagnosis, and targeted management of posterior auricular nerve disorders. The continuous advancements in diagnostic imaging technology, such as high-resolution MRI and functional imaging techniques, allow healthcare professionals to obtain more detailed information about the structure and function of the posterior auricular nerve.
By utilizing these advanced imaging techniques, healthcare professionals can better assess the integrity of the nerve, identify any abnormalities or lesions, and develop personalized treatment plans tailored to each patient’s specific condition.
Furthermore, ongoing research aims to unravel the intricate mechanisms underlying the posterior auricular nerve’s role in sensory perception and motor functions. Understanding the molecular and cellular processes involved in nerve regeneration and function can provide valuable insights into the development of targeted therapies and interventions.
Additionally, researchers are exploring the potential impact of lifestyle factors, such as diet, exercise, and environmental factors, on the health and function of the posterior auricular nerve. By identifying modifiable risk factors and protective factors, healthcare professionals can develop comprehensive strategies for preventing or managing posterior auricular nerve disorders.
In conclusion, understanding the function and importance of the posterior auricular nerve provides vital insights into its role in sensory perception, motor functions, and overall health. Seeking appropriate medical advice and treatment from healthcare professionals is essential in cases of any suspected posterior auricular nerve disorders. With ongoing research and advancements, we can expect future breakthroughs that will further enhance our understanding and management of this complex neural component.
Leave a Reply